Root canal treatment under a microscope (endodontics)
Dentysta stomatolog Warszawa Ursynów ADENTIS / Services / Root canal treatment under a microscope (endodontics)
A trivial problem? DARK TOOTH /HOLE IN THE BONE/ YOU MAY LOSE A TOOTH
Few people probably pay attention to the slightly changed tooth color! Don’t wait, REACT.
Ask your dentist to check such a tooth! The tooth may change color because it is dying. Our patient was referred for endodontic treatment.
If the doctor manages to fill the tooth properly, there is a good chance that the hole in the bone will heal.
That is, it will disappear and the bone will regenerate there. However, if this does not happen. Surgical measures will be necessary!
Therefore, be vigilant, the best dentist is yourself because you see yourself every day!
 |
“You can only treat what you can see”Professor Kim from Pennsylvania, USA Microscope in Adentis.A microscope is necessary during treatments:
In all these cases, the microscope significantly increases the chances of proper treatment, and thanks to this, the tooth can be saved from extraction. |
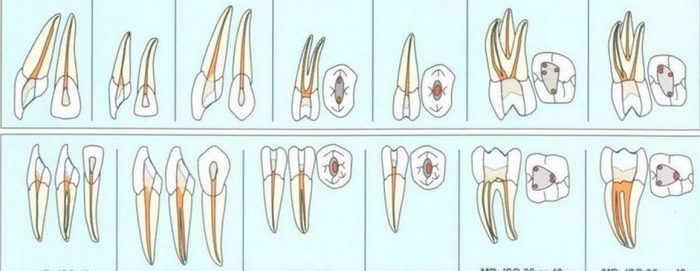
 The microscope has been found recently used in dentistry. By working with dental loupes and under a microscope, the dentist can use the magnification and illumination of the treatment area, which allows finding previously undetectable structures, visualizing root canals, and noticing narrowings, obliterations and perforations. Dental treatment becomes more precise and accurate thanks to magnification up to 25x. The inside of the tooth is a 3×4 mm hole. On this small surface in the tooth there are several root canal openings with a cross-section of just a fraction of a millimeter, which need to be found, prepared and filled. By working under a microscope, we can see the inside of the tooth at high magnification and thus work effectively.
The microscope has been found recently used in dentistry. By working with dental loupes and under a microscope, the dentist can use the magnification and illumination of the treatment area, which allows finding previously undetectable structures, visualizing root canals, and noticing narrowings, obliterations and perforations. Dental treatment becomes more precise and accurate thanks to magnification up to 25x. The inside of the tooth is a 3×4 mm hole. On this small surface in the tooth there are several root canal openings with a cross-section of just a fraction of a millimeter, which need to be found, prepared and filled. By working under a microscope, we can see the inside of the tooth at high magnification and thus work effectively.
 |
 |
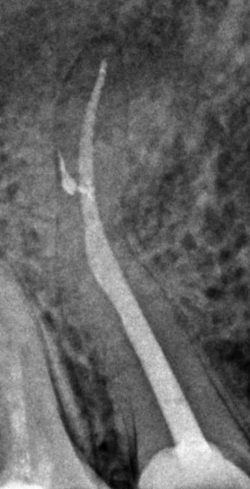
| The patient presented with a retained instrument in the lumen of the tooth canal, which prevented proper endodontic treatment of the tooth. Under the microscope, the tool was removed from the canal and the tooth was properly treated | Root canal treatment under a microscope is very helpful, especially when the tooth anatomy is different than usual. Occasionally it happens that the upper four have three channels (normally it has two). The most important thing in such situations is the experience, skill and eagle eye of the endodontist. It is a combination of two worlds – micro and macro. |
 |
 |
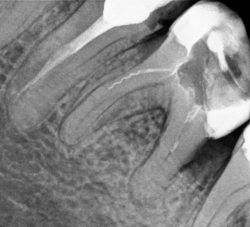
| The photo shows a properly endodontically filled tooth with periapical changes – such a filling can save and preserve the patient’s tooth for years. Before and after revision of endodontic treatment. |
The periapical lesion was caused by filling only one canal, the second canal was found under the microscope – the endodontic treatment was revised and both canals were completely filled. Follow-up X-ray taken after a year. |
 |
 |
 |
| Additional channel in top 4. | Additional channel in top 6. |
The root system in a tooth varies from person to person, so the best option for proper root canal treatment is under a microscope.
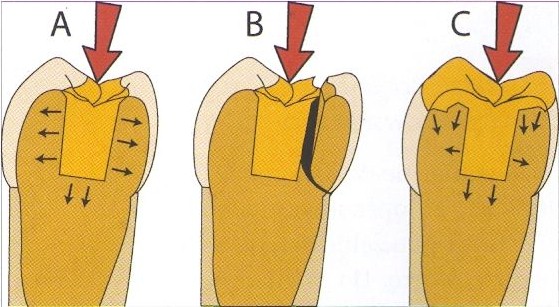
If there is too little hard tissue left after root canal treatment, it is necessary to strengthen the tooth.
The most recommended method is to rebuild the tooth covering the upper surface of the tooth, i.e. the chewing surface. This will protect the tooth against possible breakage.
Root canal treatment under a microscope.
The number of root canal treated teeth with cusps that survived in the mouth and did not break is six times greater than those that did not have chewing cusps. i.e. upper ones. Therefore, leaving the tooth without covering the cusp should be carefully considered.
This applies especially to upper premolars, where the size of the tooth crown causes thin tooth walls to remain susceptible to fracture after root canal treatment.
- A tooth with a wall thickness greater than 2 mm may be considered and possibly left without covering the chewing surface. We consider it individually.
- However, a tooth with a wall thickness less than 2 mm may be at risk of fracture in the future. Reconstruction with cusp coverage should be performed.
 |
 |
| Tooth wall less than 2mm. | Measurement with a special tool. |
 |
 |
 |
Tooth anatomy is complex and varies from patient to patient. Teeth may have more than the standard number of canals, and sometimes only the use of a microscope allows the discovery of additional canals.
 |
 |
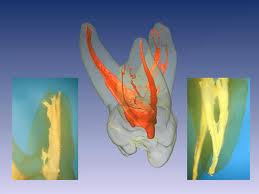 |
| Before treatment. | After endodontic treatment. | Root system. |
External resorption caused by malocclusion – overload injury.
A mucosal flap was exposed and the defect was prepared with simultaneous endodontic treatment.

Removing tools from the canal lumen under a microscope.
 |
 |
. |
 |
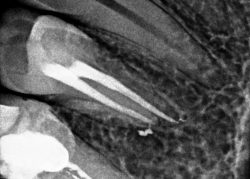
Endodontic treatment without a microscope is sometimes impossible due to:
- narrow channels,
- obliterated (unclosed) channels,
- curved roots,
- removal of root inserts,
- revision of root canal treatment.
Removal of the old post under a microscope and revision of the endodontic treatment in the rubber dam, then proper filling of the canal.
External resorption in the tooth, closed with MTA cement.
 |
 |
| Periapical lesion | The change has rolled back |
CBCT (cone cone computed tomography)
is a fast and safe version of conventional CT (computed tomography) created for dentistry. The use of cone-beam radiation allowed imaging of the facial skeleton during only one rotation of the radiation source. This results in a lower radiation dose compared to spiral tomography and a significant reduction in examination time.
A very important and valuable feature of CT is the imaging of both soft tissues and bones. No other additional test offers this possibility. The image is visible in three dimensions.
At Adentis, during endodontic treatment, the examining physician uses a CbCt test when necessary. Below are periapical lesions.
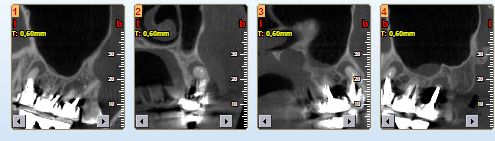
The material was resorbed in the canal lumen and inflammation occurred at the apex. Revision of root canal treatment under a microscope. The second canal was found and both canals were successfully filled. After a year, a follow-up X-ray was performed and the periapical lesion regressed.
 < /td> < /td>
| 
|
| Tooth reendo. | Tooth after filling again. |
Endodontics
 Root canal treatment, also known as endodontic treatment, is the treatment of a tooth whose pulp is inflamed or the tooth has been broken. This is then the only option to save your tooth and you should use all possibilities to keep the tooth in the mouth. There is no alternative to root canal treatment, only removal of the painful tooth. About 90% of endodontically treated teeth remain in the mouth for as long as living teeth.
Root canal treatment, also known as endodontic treatment, is the treatment of a tooth whose pulp is inflamed or the tooth has been broken. This is then the only option to save your tooth and you should use all possibilities to keep the tooth in the mouth. There is no alternative to root canal treatment, only removal of the painful tooth. About 90% of endodontically treated teeth remain in the mouth for as long as living teeth.
What does it mean that a tooth requires endodontic (root canal) treatment?
The aim of root canal treatment is to preserve the treated tooth by removing the pulp infected with dangerous bacteria, which fills the inside of the tooth and the root canals. Bacteria from the dead pulp penetrate beyond the root tips, causing inflammation of the bones and soft tissues, i.e. periapical change, i.e. bone loss around the root tip. Bacteria traveling with the blood can settle in joints, heart, kidneys, eyes and other organs. Inflammation of the tooth pulp may also lead to purulent conditions in the facial area and swelling of the face.
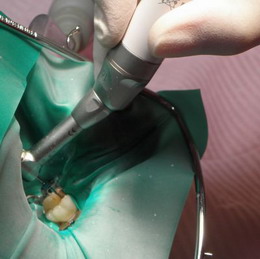
In order to effectively perform endodontic (root canal) treatment, all necessary hygienic procedures must be performed, i.e. tooth cleaning – so that plaque bacteria cannot penetrate the open tooth canals. The entire endodontic treatment (root canal) to be successful requires time and precision as well as the use of specialized diagnostic and treatment devices.
The entrances to the canals are very small and often invisible, they are located under the magnification of treatment loupes. The length of the root canals is measured with a precise electronic device – an endometer and, additionally, a digital X-ray. The canals are cleaned of dead, infected pulp using precise tools. Concentrated solutions of disinfectants are used to rinse them and kill various bacteria. Such a procedure during 9-channel endodontic treatment ensures the possibility of removing the inflammation and preserving the tooth. The X-ray shows proper root canal treatment. The white filling of the canal, contrasting with the tissue, reaches to the root tips. The tooth crown is then rebuilt. Thanks to this, the tooth is preserved and its function restored.
BeeFill – a VDW device for filling canals with liquid gutta-percha. BeeFill ensures tight, durable and hygienic filling of canals. Thanks to the latest technology, we can completely fill root canals. The VDW company has perfectly adapted the device to medical needs, thanks to it it is possible to seal the apical foramen withhot gutta-percha together with the lateral root canals.
A dam is a thin sheet of natural latex or latex-free rubber used to isolate teeth during dental procedures. The use of a rubber dam ensures the best results during dental treatment by:
•creating an aseptic barrier
• maintaining high dryness of the operating field, unavailable by other methods
• increased access to the surgical field
•increased visibility of the surgical field
 |
 |
| Root canal treatment in rubber dam | Rootally treated tooth in a rubber dam |
The success of root canal treatment depends on the proper reconstruction of the tooth walls during root canal treatment. During root canal treatment, the strength of the tooth is reduced and it may break. That is why the reconstruction of tooth walls is so important. During treatment, you should be careful when eating until the tooth is finally restored. You should not chew gum. Before root canal treatment, it is advisable to remove tartar and bacterial plaque, because the bacteria contained in the bacterial plaque may penetrate into the canal of the treated tooth, which reduces the chance of correct root canal treatment. The final reconstruction of the tooth should be started no later than 2-3 weeks after the start of root canal treatment.
 |
| 4 channels – image visible in the intraoral camera |
Stages of root canal treatment:

1. Diagnosiss
At this stage, we take an X-ray (digital technique). We assess the state of destruction of tooth tissue, the number of roots, the course and width of the canals inside each root.
2. Removal of caries from the tooth crown
We thoroughly clean the tooth, finding the entrance to the canals of all the roots.
3. Cleaning infected canals from bacteria and preparing the canals
Determining the length of the canals: with an endometer and digital radiovisiography. Removal of infected pulp from the canals (manually or machine) and chemically. Development of wide channels.
 4. Tight filling
4. Tight filling
We fill the prepared channels with material that protects them against re-entry of bacteria. After filling the canals, we take a control X-ray.
5. Permanent tooth reconstruction
Depending on the indications, we install a cosmetic composite filling or prosthetic tooth reconstruction.
Tooth reconstruction after root canal treatment
After root canal treatment of side teeth, reconstruction with a composite filling is sometimes impossible because the loss of tooth tissue is too great. Then the best way to preserve the tooth after root canal treatment is prosthetic reconstruction with ceramic overlay. This applies especially to molars and premolars, which are involved in the chewing process, which causes high forces acting on the tooth. If the tooth has little natural tissue, it may cause stress and breakage of the tooth wall. Correct tooth reconstruction after root canal treatment guarantees success in root canal treatment.
 |
|
| The plaster model shows the prepared cavity | Composite input – work on the model |
Periapical lesion
A periapical lesion is a dark spot visible on X-ray around the root tips, in which irreversible inflammation of the tooth pulp has occurred.
Periapical lesion
 |
 |
 |
 |
 |
 |
 |
| Before treatment. | After treatment. | Follow-up X-ray after 1 year. |
 |
 |
| Before treatment. | X-ray one year after treatment. |
In the lumen of the tooth canal, the material was resorbed and inflammation occurred at the apex. Revision of root canal treatment under a microscope. The second canal was found and both canals were successfully filled. After a year, a follow-up X-ray was performed and the periapical lesion regressed.
A periapical lesion is a sign of inflammation of the bone, which defends itself against the penetration of bacteria and poisons resulting from the putrefaction of the pulp, i.e. gangrene, from the root. This condition can last for years without major symptoms, but only as long as the human defense mechanisms win the fight against bacteria.
However, when microbes begin to dominate, the inflammation worsens and turns into a very painful abscess. There is swelling of the gums around the diseased tooth and even swelling of the face and fever. There is severe pain when biting the tooth or in contact with heat.
Quick root canal treatment gives a chance to save a tooth even in such a serious condition. However, it is more beneficial for health to detect periapical lesions or gangrenous teeth before they start to hurt.
Dental pulp diseases can lead to inflammation around the tooth root, which ultimately leads to periapical changes. Many years of failure to take panoramic X-rays may lead to the growth of the periapical lesion and the resorption of tooth roots (pathological root atrophy).
That’s why at theADENTISCenter, each patient has a digital panoramic radiograph. The chance of complete recovery is then much greater. Periodically performed X-rays (e.g. panoramic radiographs) are of fundamental importance in the early detection of chronic inflammation caused by gangrene of the pulp, which often function as the so-called inflammation spots
Root canal treatment
Contrary to popular opinion, root canal treatment is not a painful, long-lasting and uncertain procedure. It is performed to save a tooth that would otherwise have to be removed. After proper strengthening, a root canal treated tooth looks like a healthy, living tooth.
Root canal treatment is performed in two situations:
1. As part of a dental emergency, i.e. in situations where the tooth hurts due to pulp inflammation, gangrene, exacerbation of periapical lesion or pulp injury caused by trauma.
Characteristic ailments:

- severe sensitivity to cold or heat
- spontaneous pain that gets worse in the evening or at night
- severe pain when biting or even touching
- swelling of surrounding tissues
2. As part of comprehensive treatment, in the case of necrosis, gangrene, periapical changes, or in the case of very damaged or broken teeth, as a preliminary to prosthetic tooth reconstruction.
Characteristic features:
- no acute pain
- discoloration of an apparently healthy tooth without any external cause
- occurrence of gingival fistula (rare)
- periapical lesion visible on X-ray

